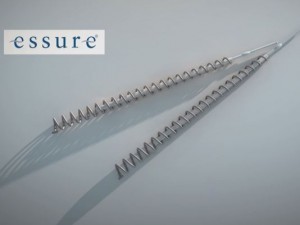
“Essure is an important permanent birth control option with a positive benefit-risk profile.”
– Bayer press release, Feb. 29, 2016 (emphasis added)
 Bayer has been defending its permanent birth control device Essure with this deceptively simple phrase positive benefit-risk profile since it started gaining bad press in the past couple years.
Bayer has been defending its permanent birth control device Essure with this deceptively simple phrase positive benefit-risk profile since it started gaining bad press in the past couple years.
What does a positive benefit-risk profile actually mean? It’s simple: A medical device has a positive benefit-risk profile if the benefits patients receive from the device outweigh the risks of the device.
For Essure’s positive benefit-risk profile to hold true, the benefits women receive from Essure should outweigh the risks of Essure.
What are some of the benefits of Essure?
- Avoiding pregnancy without hormones
- Not having to maintain a birth control regimen
- No initial surgery
What are some of the risks of Essure?
- Heavy or irregular menstrual cycles
- Allergic and autoimmune reactions
- Device migration
- Perforation of organs
- Broken or missing coils
- Pregnancy, ectopic pregnancy
- Chronic pelvic pain
- Hair loss
- Painful intercourse
- Need for surgical removal of the device, hysterectomy
Do the benefits outweigh the risks? Probably not to the thousands of women whose lives have been turned upside down because of this device.
But in the eyes of Bayer and the U.S. Food and Drug Administration, the benefits do outweigh the risks. And because they do, Essure is able to remain on the market, albeit with a stricter black box warning and mandatory patient decision checklist.
 To understand how a device as controversial as Essure can remain on the market, it helps to understand how the FDA determines the benefits and risks of a device.
To understand how a device as controversial as Essure can remain on the market, it helps to understand how the FDA determines the benefits and risks of a device.
Just this past June, the FDA released a draft guidance detailing the factors the agency considers when determining a medical device’s benefit-risk profile.
The guidance details the steps the agency takes when it finds a medical device or manufacturer is not in compliance, not the steps the agency takes when determining a device’s benefit-risk profile during the approval process.
When determining a device benefit, the FDA looks at:
- Type of benefit(s) – what positive impact does this medical device have on a patient’s health?
- Magnitude of benefit(s) – the degree to which patients experience the treatment benefit or effectiveness of the medical device
- Likelihood of patients experiencing one or more benefits
- Duration of effects – how long patients are expected to experience the benefit
- Patient preference on benefit – the value patients place on the use of the medical device
- Medical necessity – considered if the medical device provides benefits or addresses needs unmet by other medical devices or therapies
When determining risks, the FDA looks at:
- Risk severity – categorized into three levels: device-related deaths and serious injuries; device related non-serious adverse events; device-related events without reported harm. The duration of harm is also considered in risk severity.
- Likelihood of risk – a combination of the likelihood a device will have problems, the likelihood a patient will experience harm, and the total number of patients exposed
- Duration of exposure to population – the length of time between initial exposure and the point at which the harm is successfully addressed
- Patient tolerance of risk – the concern patients have regarding harm or potential harm caused by the device
Other factors include:
- Uncertainty – the degree of certainty of the benefits and risks of a device
- Mitigations – actions taken by the manufacturer or FDA to recover benefit, limit risk or limit harm
- Patient impact – the impact on the health and quality of life of a patient
- Preference for availability – Do patients prefer to have access to the device and do they understand the benefits and risks of the device?
In the guidance, the FDA explained that benefits and risks can change over time, and factors considered early in the device’s product life cycle may be reassessed as the device is used more widely.
Essure seems like a good example of how benefits and risks can change over time. The device performed well in the short-term, pre-market clinical trials commissioned by the device’s manufacturer at the time, Conceptus Inc.; but its use in the real world seems to show otherwise.
The FDA received nearly 10,000 reports of adverse side effects related to Essure between the time the device was approved in 2002 and December 2015. Adverse effects included headache, fatigue, weight fluctuations, allergic reactions, migration of the device, breakage of the device, unexpected pregnancy, and even death.
Tens of thousands more women have joined various Essure support groups on Facebook and elsewhere online and, still, Essure remains on the market.
Even though Bayer and the FDA stand by the positive benefit-risk profile of Essure, women can make that determination for themselves.
Bayer recently updated the labeling of Essure to include a black box warning and patient decision checklist. You can see how the new label compares to the old one and what those changes might mean to you here.
Free Case Evaluation
Contact Us today for a FREE, Immediate Case Evaluation
Contact Us today for a FREE, Immediate Case Evaluation
Categories
Recent post
- When Pet Owners Fail to Control Aggressive Dogs: Legal Options for Bite Victims in California
- Rideshare Driver or Passenger? Legal Steps to Take After a California Uber or Lyft Accident
- Crosswalk Accidents: When California Drivers Fail to Yield and Pedestrians Pay the Price
- Parents, Teens, and Texting: Addressing the Dangers of Distracted Driving Among Young Drivers in California
- California Rideshare Accidents Involving Minors: What Parents Need to Understand






